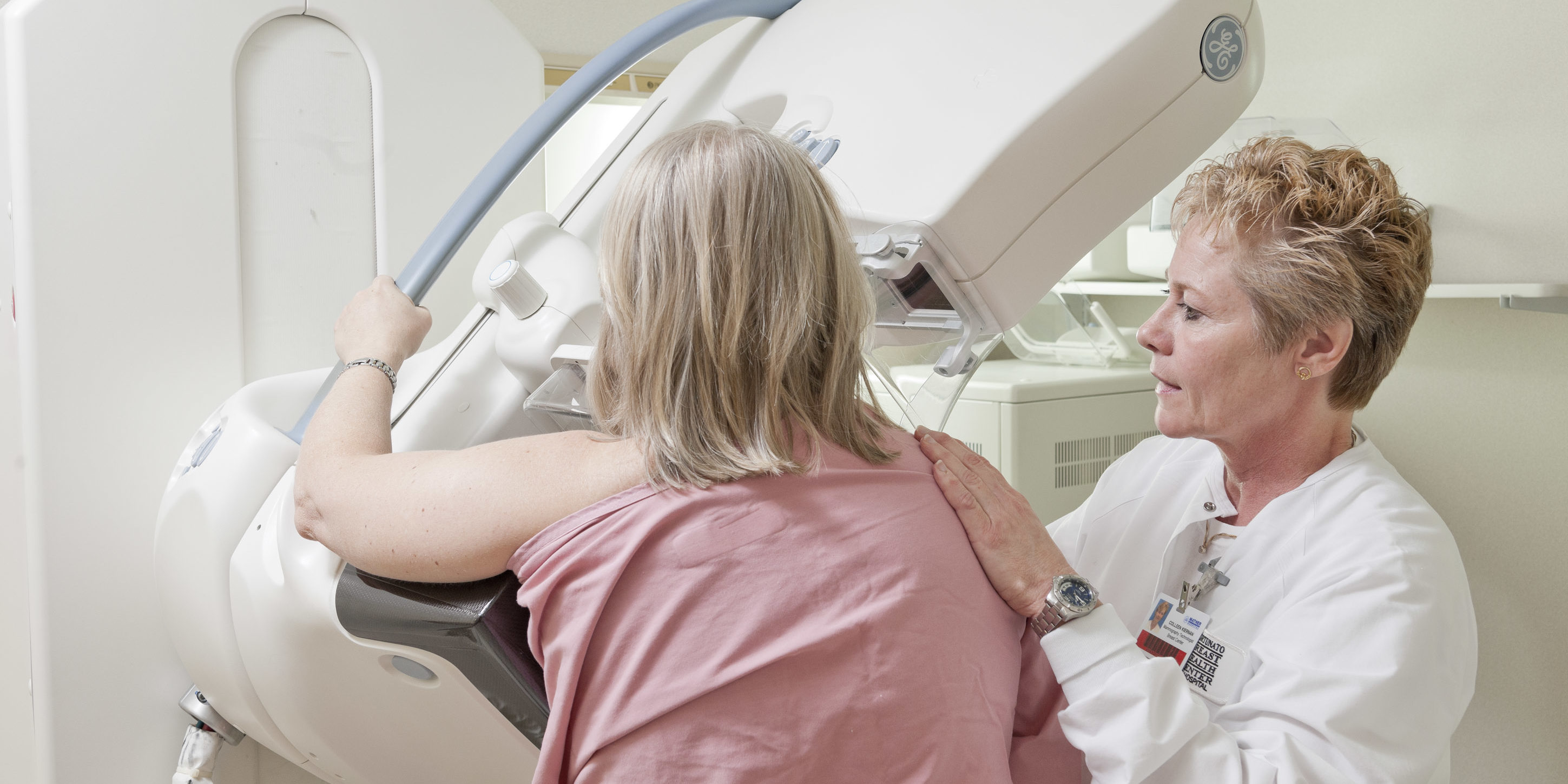
The American Cancer Society released new guidelines this week regarding mammography screening that have sparked great discussion among medical professionals. Michelle Price, MD, co-medical director of the Fortunato Breast Health Center, provided some insight into the discussion:
The American Cancer Society released new guidelines this week regarding mammography screening that have sparked great discussion among medical professionals. Michelle Price, MD, co-medical director of the Fortunato Breast Health Center, provided some insight into the discussion:
“Keeping it simple, women should undergo annual screening mammography starting at age 40. This is the recommendation at the Fortunato Breast Health Center, and it has not changed since its inception in 1999. Most other professional societies involved with the diagnosis and treatment of breast center also continue to recommend annual screening mammography starting at age 40, including the Society for Breast Imaging, American College of Radiology, and American College of Obstetrics and Gynecology, to name a few.
“The American Cancer Society reaffirms that mammography saves lives. The new guidelines suggest a more individualized approach regarding whether to screen between the ages of 40 and 45. There are several problems with implementing this approach. Young women are very busy and often do not have the opportunity to discuss in detail the pros and cons of breast cancer screening with their doctors. Different messages in the media continue to muddle the picture for women, creating a confusing scene. But even worse, most women are unaware that 75% of women diagnosed with breast cancer have no family history.
“The fact is, ALL women are at risk. All women can benefit from mammography screening and early detection. Women with additional risk factors such as dense breast tissue and family history can benefit from additional screening methods including breast ultrasound and breast MRI.
“The reported “downside” to early mammography screening involves a phenomenon known as a “false positive.” If a woman has a mammogram that shows an area of concern, she is called back for a more detailed examination of the area in question. This may include special mammography views and ultrasound. Approximately 10 percent of women screened may need this additional workup. Sometimes a biopsy is recommended. If a woman in this situation has a biopsy, and the abnormality is shown to be NOT cancer, she is in the “false positive” category. This situation applies to 1-2 percent of patients screened.
“Some organizations such as the US Preventative Task Force report that undergoing a workup with benign results causes mental stress to patients. Certainly it is stressful to need additional testing and sometimes a biopsy, but the downside of a period of stress should be compared with the potential upside of an early stage cancer diagnosis, which offers a woman her best chance at survival. From extensive experience with our patients, we find that women are willing to endure a brief period of stress if it could be a life-saving choice.
“There is no question that an earlier stage diagnosis offers the best prognosis. Mammography can detect small breast tumors years before they can be felt. Since we do not yet have a way to protect against developing breast cancer, early detection remains our best tool. Women can take a positive step in maintaining their breast health by undergoing annual mammography screening beginning at age 40.”